Q&A on Contact Tracing during COVID-19
I've received several requests to provide an overview of contact tracing generally and COVID-19 challenges particularly. This blog post serves as my responses to three important questions that have been raised. Readers should feel free to reuse and quote passages while providing appropriate attribution.
Q: How important is contact tracing in the public health response to COVID-19?
A: Case investigation and contact tracing, two related but distinct activities, are a core public health function for communicable diseases, such as COVID-19. Case investigation reveals the who/what/where/when as a person becomes ill and importantly, identifies those who may be at risk for developing disease based on contact with that person. Depending on the characteristics of the pathogen and mode of transmission, such contacts may be intimate (such as sexual or injection drug use partners) or proximate (people close if by droplet or people sharing same airspace if airborne). For COVID-19, we are specifically interested in close contacts, currently defined by the CDC as at least 15 minutes within 6 feet or closer of an individual, regardless of mask status. There is nothing magical about the 15 minute or 6 foot thresholds -- these are based on cut points in distributions and hypothesized zones of importance - and someone certainly could get ill at 7 feet distance or 14 minute duration, but these thresholds are easy to apply and somewhat intuitive. For one of these close contacts to be considered at risk, the interaction must have occurred within the infectious window of the pathogen. For SARS-CoV-2, the viral cause of COVID-19, the infectious window follows a 3-5 day incubation period and precedes illness onset (when symptomatic) by a day or two. In this respect, it is more difficult to identify than an illness such as ebola where the infectious and symptomatic periods align: that is, for ebola, individuals are only contagious when they show symptoms. Further, with asymptomatic transmission, it complicates the picture further as the exact infectious window is harder to determine. Contact tracing is so important to disease control that it is one of the first concepts taught in most outbreak investigation classes, and next to a generalized quarantine, such as a shelter-in-place order, it is probably the most effective tool public health employs during a pandemic.
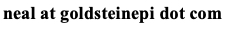
The following flowsheets from the U.S. Centers for Disease Control and Prevention depict the relationship between case investigation and contact tracing, and the steps necessary to carry out each activity. These charts represent a generalized view and individual health departments may tailor as they see fit.
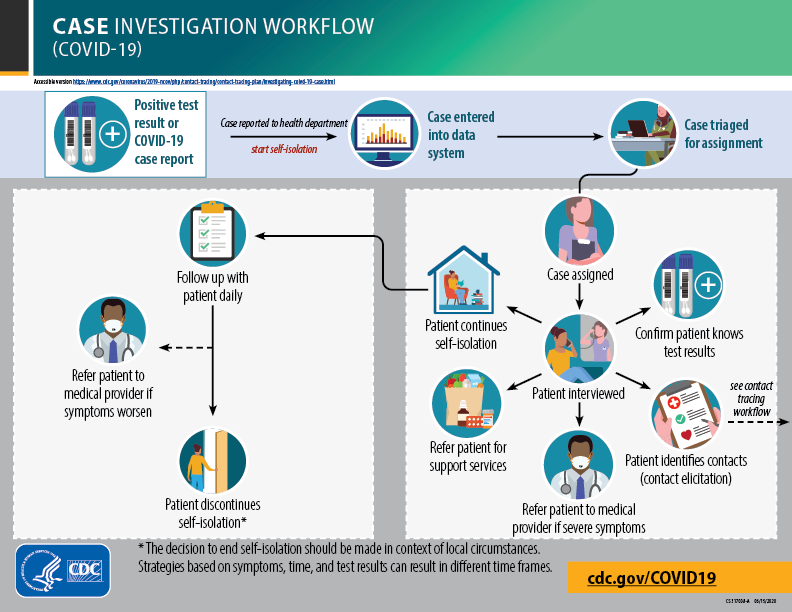
Reprinted from https://www.cdc.gov/coronavirus/2019-ncov/php/contact-tracing/contact-tracing-plan/investigating-covid-19-case.html.
Q: What is needed to make contact tracing effective?
A: This can be thought of in terms of two categories of needs. The first category is health department resources. The obvious first and foremost need is personnel. Typically, case investigators are epidemiologists who have received special training in outbreak investigation. In reality, during a pandemic where many more contact tracers are needed than available epidemiologists, almost anyone can serve in a contact training capacity, provided they have sufficient training, both in terms of contact tracing and basic epidemiology to ensure they understand terms like "exposure," "risk," "quarantine," and so on. Training programs such as those provided by the Association of State and Territorial Health Officials for new contact tracers have been key in this regard. There also is no substitute for experience as a contact tracer as eliciting contacts from a person is a delicate area. One way to view this is to make the interviewee feel as if the contact tracer is not there to obtain data, they are there to help them get through a difficult time. In reality, though, they are there to do both, as data form the backbone of the public health response. An additional resource needed is the capacity to test individuals and provide test results in an expedient manner (hours to days as opposed to weeks). Time is of the essence for a rapidly spreading respiratory pathogen, such as SARS-CoV-2. It unfortunately does little good to receive test results several weeks later: they become nothing more than historical record rather than actionable public health information. If the capacity to test is less than the demand, then public health may need to consider alternative strategies. For example, in the early pandemic in the U.S. during March and April 2020 the capacity to test was much lower than the demand, and as such, a generalized quarantine (aka "shelter in place" or "stay at home" order) was employed.
The second category is public trust and acceptance of the contact tracing program. There needs to be clear, consistent, and transparent communication about the function of contact tracing and case investigation occurring by the health department. From a typical citizen's perspective, they are receiving an often unwanted phone call from someone they have never met before asking them potentially intimate questions. It is critical that the contact tracer builds a rapport during the interview. From the interviewee's perspective, there needs to be full and accurate disclosure of information and contacts. This includes valid contact information, which in many cases may be dated or lack sufficient detail. The contact tracer needs to avoid stigmatizing anyone, maintain privacy, assuring anonymity, and providing a sense of comfort. Lastly, critical to the success of these programs, the person being asked to quarantine (or isolate if they became a case) needs to have the ability and agency to do so. This entails public health providing support for food, healthcare, rent or utility bills, social support, and so on.
To provide an idea of the difficulty encountered in real world contact tracing efforts public health departments should disclose statistics of their programs. For example, the State of Delaware provides a contact tracing dashboard. Based on these data, one can appreciate just how difficult these programs are. As of this writing, almost 50% of case investigations did not yield sufficient information for contact tracing. Among those who provided contacts, less than 50% were successfully interview. Despite these challenges, at the time of writing several thousand individuals identified through contact tracing tested positive. Assuming these individuals isolated, this potentially blocked tens of thousands of additional cases.
Q: Given these challenges, does contact tracing work if only a limited number of people are interviewed or disclosing using information?
A: On the one hand, we are clearly in a harm reduction paradigm right now as it is not possible to investigate each and every infection. This is where prioritization of contact tracing becomes important, giving priority to those with a greater hypothetical number of contacts and potential for disease transmission. When resources are limited, health departments may choose to prioritize (the triage step depicted in the above workflow) the case investigation and contact tracing to those with a large number of contacts and those whose contacts may have a large number of contacts. Healthcare workers and individuals in institutionalized settings are a prime example of a priority group. Thus, contact tracing will realize its maximum benefit in these settings. While this will have a potentially large and important impact in these specific settings (such as a given hospital or nursing home) this will have little impact at the community level.
On the other hand, every little bit helps. Some simple math can help demonstrate the power of contact tracing for a multiplicatively increasing disease like COVID-19. Assume we identify a single contact who was unaware they were exposed. This individual was reached just in time before becoming sick (and infectious) and is now self-isolating. Let us assume a basic reproduction number of 3 for SARS-CoV-2. In a community of fully susceptible individuals, i.e. not immune based on previous infection or vaccination, one case can potentially lead to 3 additional cases. If we assume a reasonable serial interval (time between horizontally transmitted infections) of 4 days, then within just a few weeks, there are potentially dozens of cases! Thus blocking one upstream case has large ramifications after a short period of time.
Cite: Goldstein ND. Q&A on Contact Tracing during COVID-19. Jan 5, 2021. DOI: 10.17918/goldsteinepi.